Can anxiety cause sleep apnea? The quick answer is no, anxiety does not directly cause Obstructive Sleep Apnea (OSA). However, research reveals a significant and concerning correlation between the two conditions.
People with OSA are much more likely to experience anxiety, and the reverse is also true: anxiety often disrupts sleep quality and can make apnea symptoms feel more severe. The relationship is not about one condition directly causing the other. Instead, it reflects a strong co-occurrence where both conditions worsen each other’s impact.
Millions of people live with this reality every day, and the overlap between anxiety and sleep apnea symptoms is hard to ignore. Poor sleep, daytime fatigue, and mood changes highlight the anxiety and sleep apnea overlap, which explains why so many are searching for answers. In this article, we will look at what science says about the connection between sleep apnea and anxiety symptoms.
Why Anxiety and Sleep Apnea Are Linked
When we look at the relationship between anxiety and Obstructive Sleep Apnea (OSA), it’s easy to assume one causes the other. However, the scientific picture is more nuanced. It’s critical to understand the difference between correlation and causation.
Causation means one thing directly creates the other. Correlation simply means two things appear or occur together frequently. Research strongly points to a powerful correlation, not direct causation. OSA is primarily a physical condition involving the airway collapsing, while anxiety is a psychological or affective disorder.
So, why do they show up together so often? The evidence is compelling.
In a nationwide South Korean study published in the JAMA Otolaryngology–Head & Neck Surgery in 2019, researchers (Kim et al.) found that OSA was significantly associated with a higher incidence of affective disorders such as anxiety and depression. This link was particularly noticeable in women. This means if you have OSA, you are statistically more likely to also be dealing with anxiety.
Another study from the Journal of Research in Medical Sciences (Rezaeitalab et al., 2014) zeroed in on the severity of the connection. They reported that more than half (53.9%) of OSA patients showed some degree of anxiety, and perhaps most tellingly, two-thirds of those with anxiety suffered from severe OSA. This finding suggests that the more severe your sleep apnea is, the higher the chances are that you’ll experience anxiety symptoms.
These findings show that while anxiety doesn’t create the physical airway blockage of OSA, the two conditions frequently overlap and influence each other. They explain why many people living with OSA also struggle with daily anxiety, which leads us to a deeper question: how exactly does anxiety change your body and your sleep to make OSA symptoms worse?
How Anxiety Affects Sleep and Breathing
We’ve already established that anxiety doesn’t directly cause the physical collapse of the airway seen in OSA. However, anxiety is a powerful force that can significantly disrupt sleep quality, breathing rhythm, and how often you wake up. This influence can make underlying sleep apnea symptoms much harder to manage and feel more severe.
Here are the key mechanisms behind this connection:
The Impact of Stress Hormones (Cortisol, Adrenaline)
When you are anxious, your body activates its “fight or flight” response, flooding your system with stress hormones like cortisol and adrenaline. Even when you are trying to sleep, this hormonal surge can cause frequent arousals throughout the night. It promotes shallow, rapid breathing and irregular sleep cycles, disrupting the deep, restorative sleep OSA patients desperately need.
The Cycle of Hyperarousal and Fragmentation
Chronic worry essentially keeps your brain in a state of hyperarousal. Instead of calming down for the night, an anxious brain remains alert. This heightened state leads to sleep fragmentation, meaning you spend less time in the necessary stages of sleep and may wake up more often. Even small disturbances, like CPAP mask irritation, can feel amplified. Using comfort-focused solutions like CPAP mask liners can help reduce irritation and improve comfort for those already dealing with anxious, sensitive sleep.
Breathing Pattern Disruption
Anxiety can directly affect your breathing patterns, sometimes triggering chest tightness or hyperventilation. These changes in breathing can complicate OSA management and make it harder for the body to settle into a consistent rhythm.
As the ResMed Sleep Health Blog notes, people prone to anxiety suffer more from sleep loss, and that poor sleep then exacerbates “excessive worry,” creating a powerful and vicious feedback loop.
The experts at Verywell Health agree, noting that disturbed sleep from OSA naturally raises daytime fatigue and stress, while anxiety makes it harder to fall back asleep after an awakening. This means each condition actively worsens the other. For instance, the dryness sometimes caused by CPAP can wake you up and trigger anxiety; adding CPAP humidifiers can help minimize that dryness and promote more consistent sleep. Similarly, ensuring consistent and comfortable airflow with high-quality CPAP hoses can prevent the leaks that often trigger nighttime stress.
The key takeaway is this: Anxiety doesn’t cause OSA, but it amplifies its effects, leading to more severe fatigue, irritability, and daytime anxiety symptoms. For the best outcome, it is often more effective to treat sleep apnea and address anxiety together, rather than only focusing on one.
Does Sleep Apnea Increase the Risk of Anxiety?
The short answer is yes. While sleep apnea does not directly cause anxiety, people with Obstructive Sleep Apnea (OSA) have consistently higher rates of anxiety disorders compared to those without the condition. The evidence strongly suggests that untreated OSA is a significant risk factor for developing or worsening anxiety symptoms. Notably, this risk often increases in severity as the sleep apnea worsens.
Key Evidence Linking OSA to Anxiety
The link between OSA and affective disorders has been explored through several authoritative studies:
Higher Incidence: A large-scale South Korean study published in the JAMA Otolaryngology–Head & Neck Surgery (2019) found that patients with OSA were significantly more likely to develop affective disorders, including anxiety and depression. The study noted that women with OSA carried an even higher risk compared to men.
Severity Matters: A peer-reviewed study in the Journal of Research in Medical Sciences (2014) highlighted the severity link. Researchers reported that 53.9% of OSA patients showed some degree of anxiety, and critically, two-thirds of those patients were classified as having severe OSA. This finding underscores that as the physical airway obstruction worsens, so does the psychological burden.
Authoritative Consensus: According to the National Sleep Foundation (2025), individuals with OSA are more likely to experience anxiety, depression, and panic disorder compared to those without sleep apnea.
The Role of Severity and Diagnosis
Mild cases of OSA may present fewer psychological symptoms, but as OSA worsens, the chances of anxiety increase significantly. A study published in the Journal of Research in Medical Sciences (Rezaeitalab et al., 2014) shows that two-thirds of anxious patients also had severe OSA, underscoring the importance of timely diagnosis and treatment.
Untreated OSA contributes to anxiety symptoms through fragmented sleep, drops in blood oxygen (desaturation), and constant nighttime arousals. This chronic physical stress and lack of restorative sleep create the perfect environment for anxiety to flourish during the day.
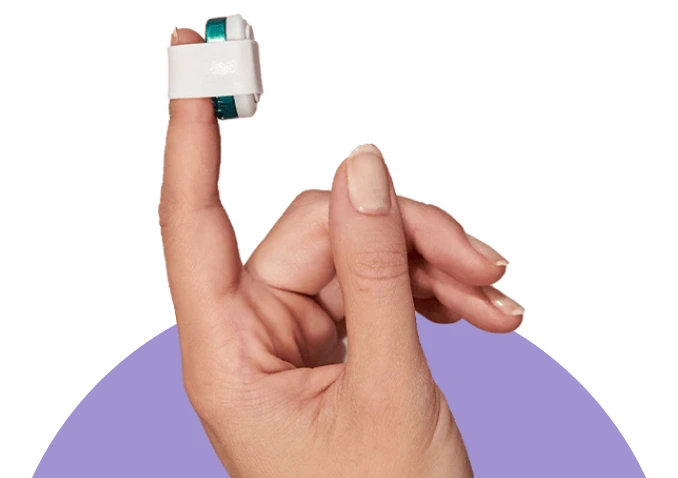
If you are struggling with both persistent anxiety and poor sleep, it’s vital to rule out an undiagnosed sleep disorder. A simple, convenient option is using a Home Sleep Study to check for undiagnosed apnea. Timely diagnosis is often the first step in breaking the anxiety-OSA cycle.
OSA Severity | Prevalence of Anxiety | Study Reference |
Mild OSA | Lower incidence | Kim et al., 2019 |
Moderate OSA | Noticeably higher rates | National Sleep Foundation, 2025 |
Severe OSA | 66%+ of anxious patients had severe OSA | Rezaeitalab et al., 2014 |
Ultimately, while anxiety doesn’t directly stem from OSA, untreated sleep apnea substantially raises the likelihood and severity of anxiety disorders. The good news is that treating the underlying OSA with Continuous Positive Airway Pressure (CPAP) therapy can often improve both sleep quality and anxiety symptoms.
CPAP Therapy and Anxiety Relief
While Continuous Positive Airway Pressure (CPAP) therapy is the gold standard for treating the physical airway obstruction of OSA, studies show it also improves sleep quality, daytime energy, and mood regulation, which can lower anxiety symptoms in patients with OSA. For many patients with co-occurring OSA and anxiety, this can lead to a notable decrease in anxiety symptoms.
The Mechanism: Restoring Deep Sleep
Consistent CPAP use works by preventing those frequent arousals that fragment your sleep and by stabilizing your oxygen levels throughout the night. By keeping the airway open, CPAP helps restore the deep, restorative stages of sleep that are essential for cognitive function and emotional regulation.
Better sleep continuity directly reduces the physical and mental stress that fuels anxiety. When you get truly restful sleep, you wake up less irritable and better equipped to handle the emotional and cognitive demands of the day. Clinical research supports this: studies often highlight CPAP’s positive impact on quality of life and mood improvements (e.g., Francisco et al. (2016), Pattison et al. (2023)).
Enhancing Comfort for Anxious Sleepers
Compliance is key, and comfort is crucial for anxious sleepers. Anything that makes the therapy feel less stressful will boost adherence.
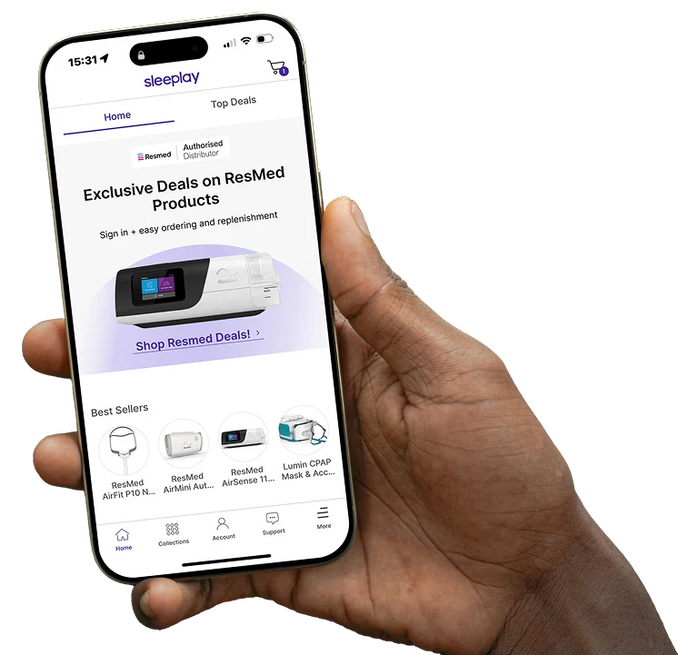
For example, machines with advanced comfort features that automatically adjust pressure to prevent jarring nighttime awakenings, such as the ResMed AirSense 11 AutoSet, can make a huge difference.
Travel can also be a major anxiety trigger, but compact devices like the Transcend Micro Auto CPAP help patients maintain consistent therapy even when away from home, removing the stress about interruptions.
Dryness and irritation are common CPAP complaints that can wake you up and trigger anxiety. Adding CPAP Humidifiers to your setup is a simple, effective solution that prevents this added discomfort.
Taking Control of Your Therapy
Feeling in control is vital for anxiety management. We offer several tools to help patients feel confident and supported:
Diagnosis: If you’re dealing with poor sleep and anxiety but aren’t diagnosed, a home sleep study is the proper first step to address both conditions together.
Mask Fit: An ill-fitting mask can cause leaks and discomfort that raise anxiety at night. Use our Mask Finder Quiz to ensure you have the best, most comfortable fit for your needs.
Tracking: Downloading the Sleeplay App allows you to track your therapy data easily, giving you a sense of control and allowing you to identify issues quickly.
Risk Check: If you are unsure of your risk for apnea, use our Apnea Risk Calculator as a quick resource.
Effective CPAP therapy reduces the physical symptoms of OSA and directly lessens emotional strain. When patients regain consistent, high-quality sleep, anxiety management often improves dramatically, marking a true turning point in their overall health.
Best Tips to Improve Comfort and Reduce Anxiety with CPAP
For people already managing anxiety, starting or continuing CPAP therapy can sometimes introduce new sources of stress. Common triggers include worrying about mask leaks, dealing with nasal dryness, or feeling anxious about the hygiene of the equipment. The good news is that these common issues are usually simple to address with a few minor adjustments and the right accessories.
Here are some practical tips to turn your nightly CPAP routine into a calming ritual:
Prevent Irritation and Leaks with Liners: Mask leaks are a major cause of sleep disruption and stress, making you worry that your therapy isn’t working. Adding mask liners provides a soft, cloth barrier between your face and the silicone. This reduces friction, prevents skin irritation, and improves the seal, helping anxious sleepers feel more secure throughout the night.
Keep Equipment Clean to Avoid Germ Anxiety: A consistent cleaning routine not only prevents bacteria buildup but also reduces the worry that poor hygiene might affect your health. Tools like the Cspring RediClean CPAP and BiPAP Cleaner make the process simple and efficient. Regular use of high-quality CPAP cleaning supplies can also help maintain both your physical health and your peace of mind.
Reduce Dryness with Better Airflow Management: Dry air can worsen anxiety by making breathing feel harder or causing irritating nasal congestion. Be sure to use your humidifier consistently. Also, replacing old CPAP hoses and tubing is important to ensure consistent, unimpeded airflow, minimizing irritation and promoting comfortable, natural breathing.
Create a Calming Bedtime Routine: Frame your CPAP setup and cleaning as part of a nightly ritual, not a chore. By integrating maintenance tasks into a quiet, relaxing routine, you reduce bedtime stress. This routine helps cue your brain that it’s time to wind down, allowing you to approach sleep with a much calmer mindset.
Comfort isn’t just about physical ease; it directly impacts your emotional well-being. Reducing small discomforts with the right accessories and routines can help you stay consistent with your therapy, significantly lowering anxiety at night.
Risks, Medications, and When to See a Doctor
While anxiety and sleep apnea often overlap, it’s important to know that certain treatments for anxiety, particularly medications, can actually complicate OSA. This makes open communication with your doctor essential when balancing your mental health care with your CPAP therapy.
The Impact of Anxiety Medications on OSA
Many medications prescribed to treat anxiety and insomnia can influence the muscles in your throat, which are already compromised by sleep apnea.
The American Sleep Apnea Association (ASAA) points out that sedatives, including medications like benzodiazepines, can relax the muscles of the throat. When these muscles relax further, the likelihood and severity of airway collapse during sleep increases, meaning your sleep apnea could get significantly worse.
Even some non-benzodiazepine sleep aids can potentially intensify breathing irregularities, making your prescribed CPAP pressure less effective. Since OSA is a physical airway issue, anything that further relaxes those critical airway muscles may increase your nightly health risks.
When to Seek Professional Evaluation
Because of this delicate balance, it is crucial to recognize when your combined treatment plan needs adjustment. Seek immediate professional evaluation if you experience any of the following:
Worsened Daytime Symptoms: If your excessive daytime sleepiness, snoring, or choking episodes become noticeably worse, especially after starting a new medication for anxiety or sleep.
CPAP Ineffectiveness: If your CPAP machine suddenly feels less effective, your mask leaks increase, or your nightly data shows a higher Apnea Hypopnea Index (AHI) despite consistent use.
Severe Psychological Symptoms: If you experience severe insomnia, chest pain, or panic attacks that emerge or worsen while you are using CPAP.
As reputable sources like the Mayo Clinic advise, professional evaluation is absolutely essential when mental health and sleep disorders intersect. Encourage your doctor to view this as an integrated treatment plan where your sleep health and mental health are managed together.
Disclaimer: This article is for educational purposes only and is not a substitute for medical advice. Always consult your healthcare provider before making changes to your medication or CPAP therapy.
FAQs
Does sleep apnea cause anxiety?
Sleep apnea does not directly cause anxiety in the way that it causes airway collapse, but the two conditions are strongly correlated. People with untreated Obstructive Sleep Apnea (OSA) have consistently higher rates of anxiety and other mood disorders compared to the general population. The physical stress, fragmented sleep, and oxygen deprivation caused by OSA create an environment in the brain and body that significantly increases the risk and severity of anxiety symptoms.
What is the link between anxiety and sleep apnea?
The link is one of mutual influence and co-occurrence. Anxiety does not cause the physical airway obstruction of OSA, but the chronic stress and hyperarousal from anxiety can disrupt breathing patterns and fragment sleep, making OSA symptoms feel much worse. Conversely, the poor sleep and physical strain of untreated OSA significantly heighten a person’s vulnerability to developing or worsening an anxiety disorder.
Can anxiety make sleep apnea worse at night?
Yes, anxiety can make the symptoms of sleep apnea feel worse at night. High anxiety levels keep the brain in a state of hyperarousal, leading to frequent micro-arousals and shallow breathing, which interfere with sleep continuity. This fragmentation, combined with stress hormone surges, complicates the body’s ability to maintain a stable airway, ultimately making the effects of your underlying OSA more noticeable and severe.
Is there a correlation between sleep apnea and panic attacks?
Yes, there is a recognized correlation between sleep apnea and panic attacks, particularly panic disorder. The sudden, brief cessation of breathing and drop in oxygen levels during an apnea event can trigger a physiological fear response, sometimes resulting in a nighttime panic attack. Furthermore, the chronic sleep deprivation and stress from untreated OSA can increase general daytime anxiety, making a person more susceptible to panic attacks overall.
How do I know if anxiety is affecting my sleep apnea?
You may suspect anxiety is affecting your sleep apnea if you experience frequent nighttime awakenings not fully explained by AHI data, have difficulty falling back asleep after a leak or minor disturbance, or feel intense stress or nervousness when you prepare to put on your CPAP mask. If you notice significantly heightened daytime fatigue and mood instability despite using your CPAP consistently, anxiety may be interfering with the quality of your therapy.
Does sleep apnea cause shortness of breath and anxiety during sleep?
Yes, sleep apnea causes brief periods of reduced breathing or shortness of breath while you sleep. The sensation of choking or gasping for air as your brain forces you to wake up to breathe can be a deeply alarming and anxiety-inducing experience. This physical event is often misinterpreted by the brain as a threat, which leads to immediate anxiety or panic upon arousal.
Can untreated sleep apnea cause anxiety in the daytime?
Absolutely. Untreated sleep apnea results in chronic sleep fragmentation, oxygen desaturation, and continuous physical stress on the body. This relentless lack of restorative sleep leaves the brain and nervous system depleted, often manifesting during the day as severe fatigue, irritability, difficulty concentrating, and heightened feelings of nervousness or generalized anxiety.
Why do I wake up with anxiety or panic while using CPAP?
Waking up with anxiety or panic while using CPAP can be due to a few reasons. Sometimes, an ill-fitting mask or a sudden air leak can create a momentary feeling of suffocation, triggering a panic response. Other times, the underlying physiological stress and lack of oxygen from a residual apnea event (if your pressure needs adjustment) or pre-existing anxiety may cause you to wake up in distress.
Does treating sleep apnea with CPAP help reduce anxiety?
Yes, treating sleep apnea with consistent CPAP therapy often helps reduce anxiety. By stabilizing oxygen levels and restoring continuous, high-quality sleep, CPAP decreases the physical stress and sleep deprivation that fuel anxiety. Patients commonly report not only improved daytime energy but also better mood regulation and a significant reduction in overall nervousness and stress.
Can CPAP therapy improve mental health symptoms?
CPAP therapy can certainly improve many mental health symptoms, particularly those related to depression, anxiety, and general mood disturbance. By addressing the root cause of fatigue and physiological stress, CPAP allows the brain to function more optimally, helping to alleviate secondary mood symptoms that were initially exacerbated by poor sleep.
What CPAP accessories help with anxiety-related discomfort (dryness, leaks, etc.)?
Several accessories can help. Mask liners reduce leaks and skin irritation, which often trigger anxiety upon waking. CPAP humidifiers prevent nasal and throat dryness that can lead to uncomfortable awakenings. Additionally, cleaning supplies and a regular maintenance routine can help reduce worries about hygiene and germs.
Should I still use CPAP if I have anxiety or panic disorder?
Yes, you should continue to use CPAP if you have anxiety or panic disorder, as consistent therapy is vital for your health. Untreated OSA can worsen your anxiety, while effective CPAP can alleviate it. It is best to work closely with your sleep doctor and a mental health professional to address any feelings of claustrophobia or panic related to mask use through a gradual desensitization process.
Can anxiety medications make sleep apnea worse?
Yes, certain anxiety medications can worsen sleep apnea. Specifically, sedating drugs like benzodiazepines work by relaxing the central nervous system, which can, unfortunately, also cause the muscles in the throat to relax excessively, increasing the risk of airway collapse and making sleep apnea more severe.
Do benzodiazepines increase sleep apnea risk?
Benzodiazepines are known to increase the risk and severity of obstructive sleep apnea. By relaxing the upper airway muscles, they destabilize the throat structure during sleep, leading to more frequent and longer-lasting apnea events. It is critical to inform your sleep physician if you are taking any medication in this class.
Are antidepressants safe if I have sleep apnea?
Antidepressants are generally considered safer for people with sleep apnea than benzodiazepines, but you must consult your doctor. Some classes of antidepressants may have sedating effects or impact REM sleep, which could theoretically affect breathing patterns. A detailed discussion with your prescribing physician is necessary to choose an option that balances mental health benefits with minimal risk to your sleep apnea.
When should I see a doctor if I have anxiety and sleep apnea together?
You should see a doctor immediately if you notice that your CPAP therapy suddenly seems less effective, if new anxiety medications worsen your snoring or daytime sleepiness, or if you experience severe symptoms like chest pain, uncontrollable panic, or persistent insomnia. These are signs that your integrated treatment plan needs urgent review.
How can I manage anxiety to sleep better with CPAP?
To manage anxiety and sleep better with CPAP, establish a relaxing bedtime ritual that includes using your machine. Practice desensitization techniques for the mask, ensure optimal comfort with accessories like liners and humidifiers, and incorporate breathing exercises or meditation before bed to calm your nervous system.
Do nasal rinses or humidifiers help reduce CPAP-related anxiety?
Yes, both can help reduce CPAP-related anxiety indirectly. Humidifiers prevent a dry nose and throat that can lead to irritating and anxiety-provoking awakenings. Nasal rinses help keep the nasal passages clear, ensuring that breathing through the mask feels easy and natural, reducing the feeling of air restriction that can trigger anxiety.
Can weight loss or lifestyle changes reduce both sleep apnea and anxiety?
Yes, weight loss and healthy lifestyle changes can positively impact both conditions. Losing weight can reduce the tissue around the airway, lessening the severity of OSA. Regular exercise, improved diet, and reduced alcohol consumption are proven to benefit overall mental health, directly easing anxiety symptoms.
How common is anxiety in people with sleep apnea?
Anxiety is very common in people with sleep apnea. Studies suggest that over half (53.9%) of OSA patients show some degree of anxiety, a rate significantly higher than in the general population. This correlation becomes even stronger in patients with severe OSA.
Are women with sleep apnea more likely to develop anxiety?
Research indicates that women with sleep apnea may have an even higher incidence and risk of developing affective disorders, including anxiety and depression, compared to men with the condition. This highlights the importance of screening women with OSA for mental health symptoms.
Can sleep apnea be mistaken for anxiety or depression?
Yes, sleep apnea is often initially mistaken for or misdiagnosed as anxiety or depression. The overlapping symptoms of daytime fatigue, irritability, poor concentration, and mood changes can be attributed to a mental health condition when the root cause is actually the physical disturbance of sleep due to OSA.