Navigating how to get your CPAP therapy gear can be a bit of a maze, right?
Most insurance plans, whether private, Medicare, or Medicaid, will typically help with the CPAP machine cost, with insurance covering a portion of your CPAP machine and essential supplies. However, this route often means dealing with paperwork, potentially starting with a rental, and adhering to strict usage rules to keep that coverage.
On the flip side, when you consider the out-of-pocket CPAP cost, buying directly gives you more say in what you get and how fast you get it, offering a wider selection of devices and a quicker setup.
The catch? It usually means a higher upfront cost, but as we’ll explore, it might not always be the more expensive path in the long run. Also, does insurance cover CPAP fully? Beyond just a yes or no, getting a more profound understanding is key to making the best choice for your sleep and your wallet.
Here’s what you’ll learn as we break it all down:
How CPAP insurance coverage works with private, Medicare, and Medicaid plans.
The typical cost of a CPAP machine with and without insurance.
What’s included (and what’s not) when using insurance
Which option may save you time or money in the long run
Let’s get started.
Quick Answer — Does Insurance Cover CPAP?
Yes, most private insurance plans, as well as Medicare and Medicaid, typically cover CPAP machines, which are classified as durable medical equipment (DME).
So, is CPAP covered by insurance? Often, yes. However, this coverage is almost always conditional.
To ensure the CPAP machine cost with insurance is actually taken care of, you’ll usually need a formal sleep apnea diagnosis from a qualified physician, a valid prescription, and you’ll have to meet ongoing compliance requirements, like proving you’re using the machine regularly.
Here’s a quick rundown of key factors when dealing with insurance for CPAPs:
Coverage type: CPAP machines, masks, tubing, and filters may be covered as essential durable medical equipment.
Out-of-pocket costs: You’ll likely still be responsible for deductibles, copayments, or coinsurance amounts set by your plan.
Equipment limitations: Be aware that some specific types of machines, such as certain auto-CPAP models or specialized travel devices, might not be covered or may require extra justification.
Usage compliance: Many insurance plans require documented proof that you’re using the CPAP machine for a minimum number of hours nightly (often at least 4 hours) on a high percentage of nights (typically 70%).
As Dr. Indira Gurubhagavatula, a sleep medicine physician at the University of Pennsylvania Health System, noted, these compliance rules can sometimes unfairly penalize patients. She points out that some individuals “may have child care or elder responsibilities that makes their sleep disrupted… The rule is arbitrary because using the machine, even if part time, is beneficial.” khn.org (Published July 17, 2019 – Source: Kaiser Health News)
Understanding these initial points is crucial before deciding which insurance route to take for your CPAP therapy.
How Insurance Covers CPAP (Private, Medicare, Medicaid)
Getting your CPAP covered by insurance isn’t a one-size-fits-all deal. It depends on the type of insurance you have. Let’s look at the common routes: private insurance, Medicare, and Medicaid, and what you can generally expect from each.
1. Private Insurance
If you have health insurance through your employer or the marketplace, here’s generally how it works for CPAP coverage:
Eligibility Requirements:
You’ll definitely need a valid prescription from your doctor. No getting around that!
A formal diagnosis of sleep apnea via a sleep study is a must. This could be an in-lab study or an approved home sleep test (HST).
Most insurers will want to see compliance with CPAP usage. This usually means using the machine for at least 4 hours per night, for at least 70% of nights, typically reviewed after the first 30 days and periodically thereafter.
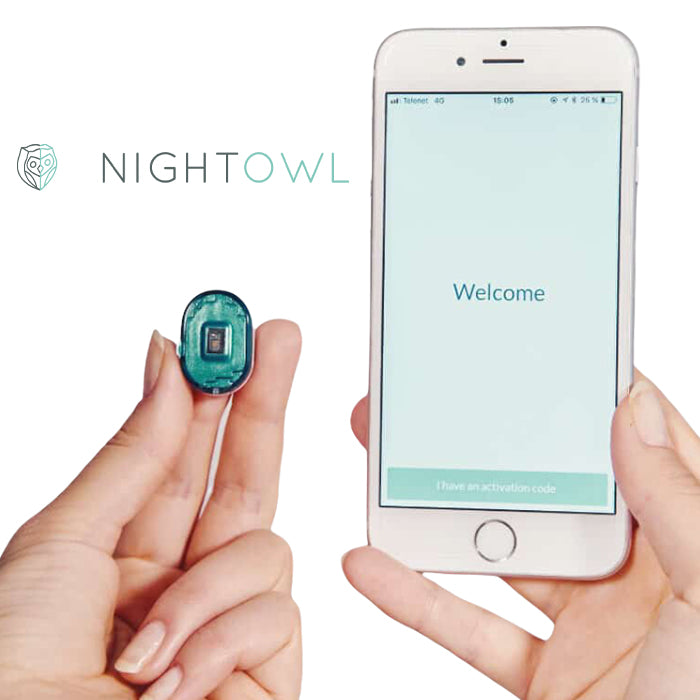
The Night Owl Home Sleep Test offers a simple, convenient, and hassle-free way to test for sleep apnea from the comfort of your own home.
$139.99
Payment Model:
Many private insurers use a rent-to-own system. You’ll pay a monthly rental fee for the CPAP machine, and after a set period (often 10-12 months), you’ll own it.
Be prepared for out-of-pocket costs. Even with coverage, you’ll likely have to meet your annual deductible first, and then you might still have copayments or coinsurance for the machine and supplies. This can be a significant hit, especially if you have a high-deductible health plan (HDHP).
Good news for those with Flexible Spending Accounts (FSA) or Health Savings Accounts (HSA): You can typically use these pre-tax funds to pay for your CPAP machine, as well as essential supplies like masks, tubing, and filters. This can help ease the financial burden.
Limitations:
Don’t expect all the bells and whistles to be covered. Many plans don’t cover extras like CPAP cleaning machines, external battery packs for travel, dedicated travel-sized CPAPs, or advanced comfort features like humidifiers.
Some insurance plans might also restrict the brands or specific models of CPAP machines they’ll cover. For example, they might prefer a standard CPAP over an auto-CPAP unless your doctor justifies explicitly the need for an auto-adjusting machine.
2. Medicare
For those relying on Medicare, CPAP coverage has its own set of rules:
Eligibility Requirements:
You must have had a face-to-face evaluation with your doctor, undergo a Medicare-approved sleep study (in-lab polysomnography or a home sleep test), and receive a confirmed diagnosis of Obstructive Sleep Apnea (OSA).
A prescription from a Medicare-enrolled physician is required.
CPAP therapy is covered under Medicare Part B as Durable Medical Equipment (DME).
Payment Model:
Once you’ve met your annual Part B deductible, Medicare generally covers 80% of the Medicare-approved amount for the CPAP machine rental.
You, the patient, are responsible for the remaining 20% coinsurance. If you have a Medicare Supplement Insurance (Medigap) plan, it might cover this 20%.
The typical rental period is 13 months. After Medicare has made payments for 13 continuous months, you’ll own the machine.
Compliance Requirement:
This is crucial: Medicare coverage only continues if you meet specific usage requirements. You must use the machine for at least 4 hours per night on 70% of nights during a consecutive 30-day period within the first 90 days of starting therapy. Your DME supplier will likely monitor this remotely.
Failure to meet these compliance standards can mean Medicare stops paying, and you might have to start the whole process over, potentially including a new sleep study and prescription, if you want coverage to resume.
As sleep apnea specialist Dr. Ofer Jacobowitz highlighted, “Patients often pay rental fees for a year or longer… and may end up covering the entire cost of the rental for much of that time” (Source: NPR.org, Nov 21, 2018), especially if compliance isn’t met and coverage is denied.
Additional Notes:
Medicare has a set replacement schedule for CPAP supplies. For example, you might get a new mask every 3 months and new tubing every 3 months.
Generally, FSA/HSA funds cannot be used directly with Original Medicare because you can’t contribute to an HSA if you’re enrolled in Medicare. However, if you have a Medicare Advantage plan, some of these plans offer supplemental benefits or accounts that might be similar, or if you have an HSA from previous employment, you might be able to use those funds for qualified medical expenses not covered by Medicare.
3. Medicaid
Medicaid coverage for CPAP therapy can vary significantly because it’s administered at the state level:
Eligibility Requirements:
As mentioned, coverage details differ from state to state.
However, common requirements usually include:
A sleep study diagnosis confirms sleep apnea.
A prescription from a Medicaid-enrolled healthcare provider.
Proof of medical necessity, which often involves your Apnea-Hypopnea Index (AHI) score from the sleep study.
Payment Model:
Many state Medicaid programs tend to follow a model similar to Medicare’s, often involving an initial trial period (e.g., 12 weeks). Continued coverage then depends on whether you meet compliance criteria.
Some states might approve an outright purchase of the CPAP machine from the start, rather than a rent-to-own arrangement, though this is less common.
Compliance & Documentation:
Medicaid typically mirrors Medicare’s compliance rules: that same 4 hours per night, 70% of nights, within a 30-day window is a common benchmark.
You might also need regular follow-up visits with your doctor, and they may need to provide updated prescriptions or documentation to Medicaid to ensure continued coverage for your machine and supplies.
Limitations:
Accessory replacement schedules under Medicaid can sometimes be stricter or less frequent than those with private insurance or even Medicare.
Some state Medicaid programs may also have more limited options for CPAP machine models or brands, potentially not covering some of the newer or more advanced devices.
A Note on HSA/FSA:
Generally, individuals whose primary insurance is Medicaid don’t typically have or use HSAs or FSAs, as these are often tied to employer-sponsored health plans or high-deductible plans, which are different structures from Medicaid. However, it’s important we mention terms like HSA for CPAP or FSA for CPAP supplies for those who are broadly researching.
For individuals who are dual-eligible (meaning they have both Medicare and Medicaid), their out-of-pocket costs for CPAP therapy can often be significantly lower, as Medicaid may cover the costs that Medicare doesn’t. In rare cases where a dual-eligible individual might also have access to an FSA (perhaps through spousal employment), those funds could still be used for any remaining out-of-pocket health expenses, including non-covered CPAP accessories.
Out-of-Pocket CPAP Costs (With Real Examples)
CPAP machines typically cost between $400 and $2,000 out of pocket, depending on the model, features, and whether it’s a standard CPAP, an auto-CPAP, or a BiPAP machine.
Many people opt to pay out of pocket for a few key reasons: there’s no need for insurer-mandated compliance monitoring or usage tracking, you often get immediate access to the device without waiting for approvals, and you have the freedom to choose premium brands and specific features that your insurance might not cover.
Here’s a quick peek at some popular models and what they might cost when you buy them directly, along with features and common insurance hurdles:
Model | Approx. Cost | Key Features | Insurance Restrictions |
ResMed AirSense 11 | $989–$1,200 | Auto-adjust, Humidifier, myAir App | Not always covered by basic plans |
ResMed AirMini | $919 | Compact, Travel-friendly | Often excluded or not reimbursed |
ResMed AirCurve 11 BiPAP | $1,800+ | Dual pressure settings, HumidAir | May require prior authorization |
It might seem counterintuitive, but going the out-of-pocket route can sometimes save you money or at least significant hassle.
You can often avoid shelling out for high deductibles before insurance even kicks in, skip ongoing monthly rental fees that can add up (sometimes exceeding the machine’s cost!), and sidestep frustratingly long delivery timelines due to insurance processing. Plus, you get full ownership of your device from day one, and there’s no risk of losing your machine or having coverage denied down the line because you didn’t meet strict, insurer-imposed usage metrics.
And if you’re looking for ways to manage these out-of-pocket expenses, some retailers offer helpful programs. For instance, at Sleeplay, you can find options designed to ease the burden, such as assistance with prescription renewals if needed (often with no extra fees), a “Subscribe & Save” program for automatic and discounted replacements of masks and supplies, cost-saving bundles when you purchase a machine and mask together, and a rewards program where you earn points with every purchase that can be used toward future orders.
Popular Machines
Pros & Cons — CPAP Insurance vs. Paying Yourself
If you’re unsure which route to take, this side-by-side comparison can help clarify the key trade-offs.
Feature | Insurance | Out-of-Pocket |
Machine Selection | Limited; may not include top models like AirSense 11 | Full access to latest models, travel CPAPs, bundles |
Machine Condition | Could be new or refurbished | Always brand new |
BiPAP Eligibility | Must fail CPAP trial (APAP) before BiPAP is approved | Immediate access if prescribed |
Fulfillment Speed | Delayed due to approvals, documentation | Fast shipping (24–48 hrs if Rx on file) |
Initial Cost | Lower upfront (may include copay, deductible) | Higher upfront, but may be cheaper long-term |
Co-Payments | Yes, varies by plan | None |
Rental Term | Usually rent-to-own (3, 10, or 13 months) | Immediate ownership |
Prescription Validity | Typically 12 months | 99 years (Sleeplay honors long-term Rx) |
Usage Requirements | 4 hrs/night, 70% of nights, tracked over 30 days | No compliance requirements |
Follow-Ups | Recertification every 6 months or annually | None |
Part Replacement | Follows insurer’s replacement schedule | Replace whenever needed |
Accessory Coverage | Limited (filters, hoses, and humidifiers may not be fully covered) | Full control over accessory purchases |
Device Customization | Standard models only | Freedom to choose features like humidification, apps, and travel size |
Data Privacy | Usage data shared with the insurer | Private use, no tracking |
Support Services | Based on supplier availability | Sleeplay offers expert support, Rx renewals, and reward points |
FSA/HSA Eligibility | Yes, typically applies | Yes, most out-of-pocket CPAP purchases qualify under FSA/HSA spending accounts |
So, what’s the bottom line? Using insurance might offer some savings on the initial cost of a CPAP machine, but it often comes with strict rules, potential delays, and fewer choices in what equipment you get. On the other hand, paying out of pocket gives you full control over your purchase, faster access to your therapy, and freedom from compliance worries, though the upfront cost is higher. Before you decide, it’s a good idea to carefully review your insurance plan’s deductible, co-pay terms, and specific device eligibility for CPAP therapy to see which option truly fits your needs and budget best.
What CPAP Supplies Are Covered (and What’s Not)
When you get your CPAP through insurance, coverage for supplies can be a bit specific. Here’s a general idea:
1. Usually Covered (Durable Medical Equipment – DME)
These items are typically seen as medically necessary and generally fall under your insurance plan’s DME coverage. Think of them as the essentials to make your therapy work:
CPAP machine
Standard tubing
CPAP mask (nasal mask, full-face mask, or nasal pillows mask)
Headgear and chin straps (sometimes limited)
Water chamber for the humidifier
Disposable filters
Non-disposable filters (varies by plan)
Oxygen sensors or Humidifier units (case-by-case)
It’s also good to know that many plans, especially Medicare and Medicaid, follow specific replacement schedules. For example, Medicare often covers new tubing every 3 months, a new mask every 3 months, and disposable filters twice per month. You can’t just order them whenever you feel like it if you want insurance to pay.
2. Not Always Covered (Optional or “Comfort” Supplies)
These items, while helpful, are often considered optional or “comfort” accessories. They are often not reimbursed by insurance and may need to be purchased out of pocket if you want them:
Knowing this helps you plan! It’s not about being penalized by limitations, but about understanding where your insurance is likely to draw the line so you can budget accordingly.
Medicare/Medicaid Notes:
Just a heads-up: Medicare has a detailed CPAP Supply Replacement Schedule that many private insurance plans also tend to follow as a guideline. You don’t need to memorize it here, but you can usually find the full breakdown on the official Medicare.gov website or by asking your insurer directly.
For Medicaid, these rules can vary quite a bit from state to state, so your best bet is to check with your state’s Medicaid plan administrator for their specific supply coverage.
A Helpful Tip:
If you find yourself needing those non-covered supplies, or if you prefer to replace items more frequently than your insurance allows, remember that out-of-pocket doesn’t have to mean breaking the bank.
Retailers like Sleeplay offer convenient out-of-pocket options for non-covered supplies, often with bundle discounts and subscription savings. It may be more affordable than trying to go through insurance for small, recurring items.
FAQs About CPAP Coverage and Costs
How much does a CPAP machine cost with insurance?
Your CPAP machine cost with insurance depends on your specific plan’s deductible, copay, and coinsurance. This means your share could be minimal or run into several hundred dollars, especially with high-deductible plans.
Does insurance cover a CPAP machine?
Yes, most health plans cover them as durable medical equipment (DME) if you have a doctor’s diagnosis, a prescription, and meet their usage rules.
How much is a CPAP machine without insurance?
Expect prices from roughly $400 to $2,000. The cost varies by the machine’s type (CPAP, APAP, BiPAP) and included features.
What CPAP supplies does insurance cover?
Insurance usually covers medically necessary CPAP supplies like masks, standard tubing, headgear, basic humidifiers, and filters. Be aware that most plans have specific replacement schedules for these items.
Does Medicare or Medicaid cover CPAP?
Yes, both Medicare and Medicaid typically cover CPAP machines and essential supplies as DME. Each has distinct eligibility criteria, often a rental period (like Medicare’s 13-month rent-to-own), and compliance requirements.
Can I buy a CPAP machine without insurance?
Absolutely, you can buy a CPAP machine without insurance as long as you have a doctor’s prescription. This route gives you more device options and frees you from insurance compliance tracking.
Is it better to pay out of pocket for CPAP?
Whether to pay out of pocket for CPAP or not depends on your situation. If you value wider choice, quicker access, and no compliance stress over a higher upfront cost, it might be. Compare your insurance terms carefully.
How do I get a CPAP machine covered by insurance?
To get a CPAP machine covered by insurance, you’ll typically need a sleep study, an official diagnosis and prescription from your doctor, and then you must use an in-network DME supplier, meeting all your insurer’s specific criteria.
What are the insurance compliance rules for CPAP?
Insurance compliance rules for CPAP usually mean you must use the machine for a minimum number of hours nightly (e.g., 4 hours) for a high percentage of nights (e.g., 70%), with usage data often tracked for continued coverage.
Will my FSA/HSA cover a CPAP machine?
Yes, your FSA/HSA will cover a CPAP machine and related supplies like masks and tubing. These are considered qualified medical expenses, making them eligible for these pre-tax accounts.
Does Blue Cross Blue Shield insurance cover CPAP machines?
Generally, Blue Cross Blue Shield insurance covers CPAP machines as DME. However, the exact coverage, costs, and requirements depend heavily on your specific BCBS plan, so always verify with them directly.
How much are CPAP machines with insurance?
The cost for CPAP machines with insurance isn’t fixed; it hinges on your plan’s deductible, copay, and coinsurance. Your out-of-pocket expense could be small or quite significant based on these.
Are CPAP machines covered by insurance?
Yes, health plans generally cover them as DME with a qualifying diagnosis and prescription, but expect specific conditions like pre-authorization or usage tracking.











